Health Lab
Michigan Medicine's daily online publication featuring news and stories about the future of health care.

Health Lab
Being named after four-time WWE Championship title holder Roman Reigns means having an innate toughness

Want top health & research news weekly? Sign up for Health Lab’s newsletters today!

Health Lab
Young heart transplant recipient develops post-transplant lymphoma, but perseveres

Health Lab
Overuse of antibiotics can lead bacteria to evolve antimicrobial resistance, but Americans are still receiving the drugs for many conditions that they can’t treat.
Health Lab
While most parents of preschool and elementary aged children strive to give their children a balanced, nutritional diet, some of their strategies to promote healthy eating may backfire.

Health Lab
Researchers recently revealed a new mechanism behind antiphospholipid syndrome that the investigators hope will eventually allow treatments to be targeted closer to the source of the problem.

Health Lab
Data on medical cannabis use found that enrollment in medical cannabis programs increased overall between 2016 and 2022, but enrollment in states where nonmedical use of cannabis became legal saw a decrease in enrollment

Health Lab
A new urine-based test addresses a major problem in prostate cancer: how to separate the slow growing form of the disease unlikely to cause harm from more aggressive cancer that needs immediate treatment.

The Health Lab Podcast
Subscribe today on Apple Podcasts, Google Podcasts, Spotify, Stitcher or wherever you get your podcasts.

Health Lab
Overuse of antibiotics can lead bacteria to evolve antimicrobial resistance, but Americans are still receiving the drugs for many conditions that they can’t treat.

Health Lab
Data on medical cannabis use found that enrollment in medical cannabis programs increased overall between 2016 and 2022, but enrollment in states where nonmedical use of cannabis became legal saw a decrease in enrollment

Health Lab
A new urine-based test addresses a major problem in prostate cancer: how to separate the slow growing form of the disease unlikely to cause harm from more aggressive cancer that needs immediate treatment.

Health Lab
Researchers recently revealed a new mechanism behind antiphospholipid syndrome that the investigators hope will eventually allow treatments to be targeted closer to the source of the problem.

Health Lab
Among people with multiple sclerosis in the United States, more than half experienced at least one fall in a six-month period and approximately one-third of those falls resulted in an injury.
Health Lab
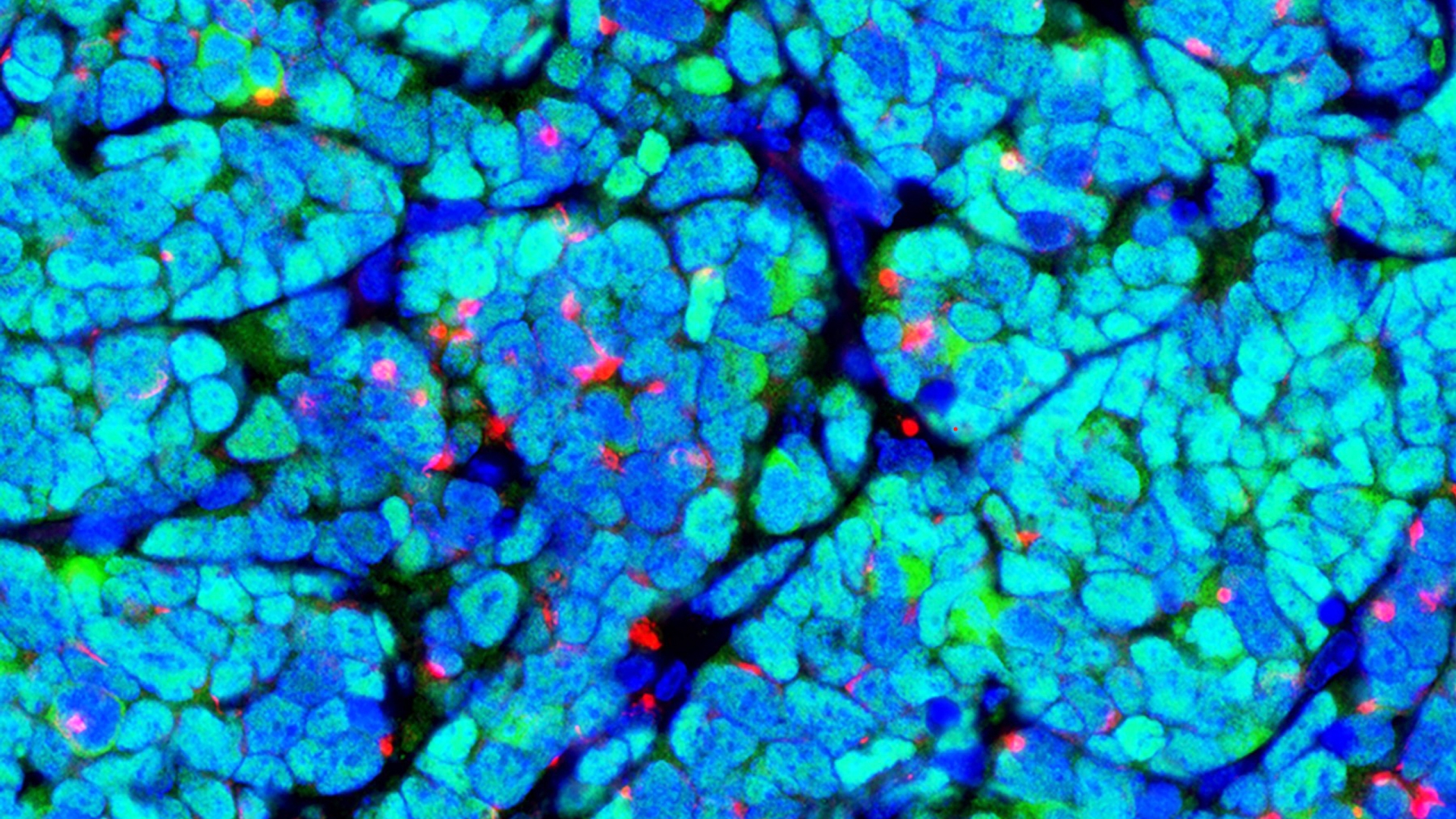
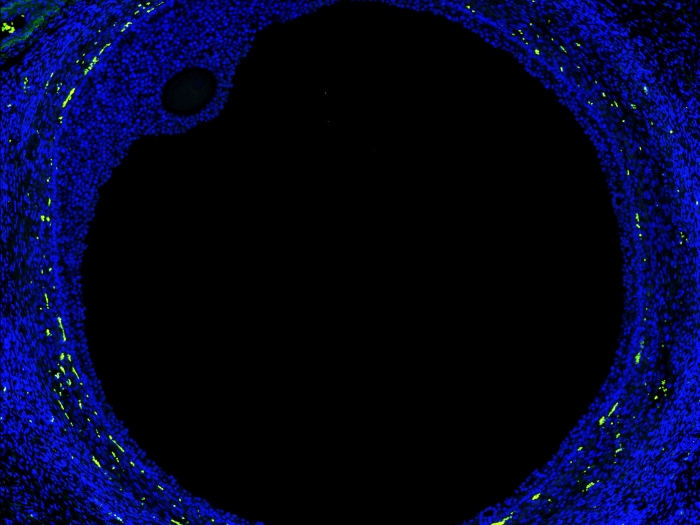
New map of the ovary provides a deeper understanding of how oocytes interact with the surrounding cells during the normal maturation process, and how the function of the follicles may break down in aging or fertility related diseases.