Health Lab
Michigan Medicine's daily online publication featuring news and stories about the future of health care.
Health Lab
Certain therapeutics, such as human cells and tissues, are only minimally regulated by the U.S. Food and Drug Administration

Want top health & research news weekly? Sign up for Health Lab’s newsletters today!

Health Lab
A JAMA viewpoint outlines the tragic story of Shandra Eisenga, a patient who received spine surgery for back pain only to inexplicably contract tuberculosis.

Health Lab
Research published in PNAS examines how the bacteria Escherichia coli, or E. coli—responsible for most UTIs—is able to use host nutrients to reproduce at an extraordinarily rapid pace during infection despite the near sterile environment of fresh urine.

Health Lab
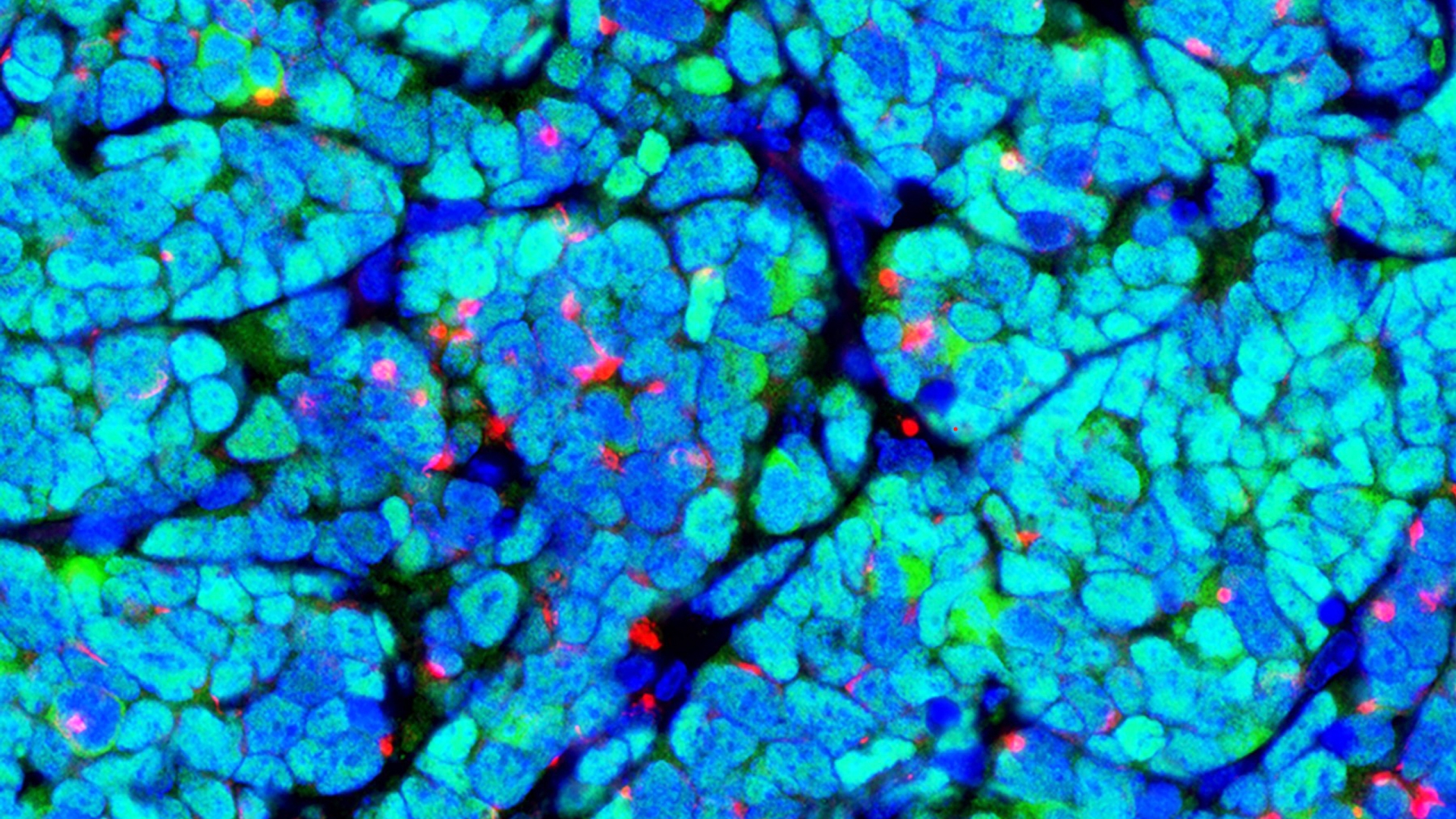
A study led by University of Michigan Health Rogel Cancer Center researchers identifies novel biomarkers in renal cell carcinomas.

Health Lab
Experts discuss pregnancy and heart health.

Health Lab
People over 50 of all backgrounds say they’re most concerned about various kinds of health costs affecting people their age, including insurance, prescriptions, medical care, dental care and home or longterm care.

Health Lab
Created by a patient and grieving parent, a peer and medically reviewed guidebook on pregnancy and infant loss offers others going through the same experience more resources during the difficult time.

The Health Lab Podcast
Subscribe today on Apple Podcasts, Google Podcasts, Spotify, Stitcher or wherever you get your podcasts.

Health Lab
Building a comprehensive human kidney cell and tissue catalog could help develop more treatments for kidney disease.
Health Lab
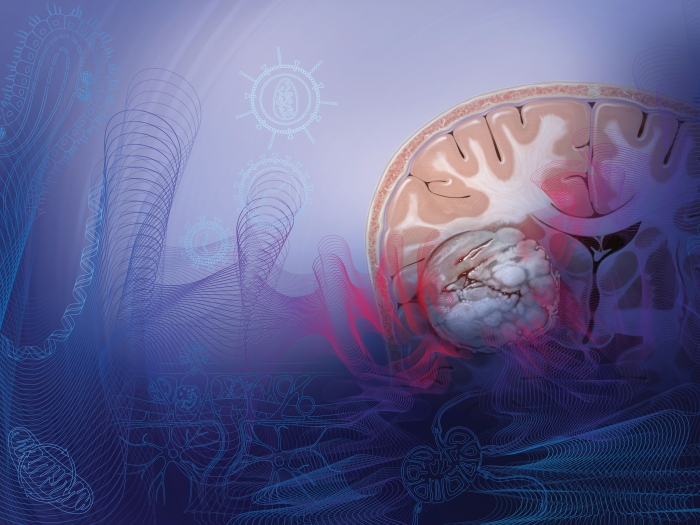
Experts in brain cancer outline current discoveries and offer a path of hope for glioblastoma treatment
Health Lab
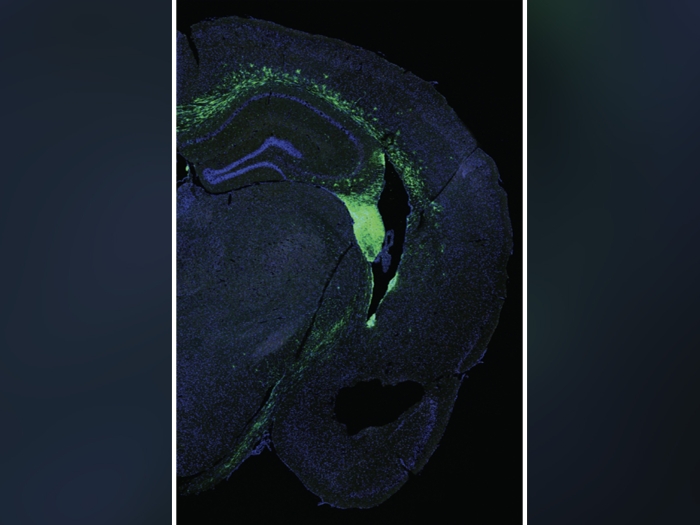
Researchers improved memory and reduced neuroinflammation in a mouse model of Alzheimer’s Disease, suggesting another avenue for potential treatment.

Health Lab
Buprenorphine prescribing for opioid addiction used to require a special waiver from the federal government, but a new study shows what happened in the first year after that requirement was lifted.

Health Lab
Researchers have used advanced computer algorithms to uncover distinct molecular subgroups of kidney diseases, independent of clinical classifications. These findings have significant implications for personalized treatment approaches.

Health Lab
Overuse of antibiotics can lead bacteria to evolve antimicrobial resistance, but Americans are still receiving the drugs for many conditions that they can’t treat.