Health Lab
Michigan Medicine's daily online publication featuring news and stories about the future of health care.
Health Lab
Many who get antibiotics in clinics and emergency departments have no diagnosis or symptoms that might explain a prescription; improved diagnosis coding could help target efforts to optimize use and reduce risk

Want top health & research news weekly? Sign up for Health Lab’s newsletters today!

Health Lab
Efforts to reduce overuse of antibiotics may be hampered by incomplete medical records that don’t show the full reasons for prescriptions.
Health Lab
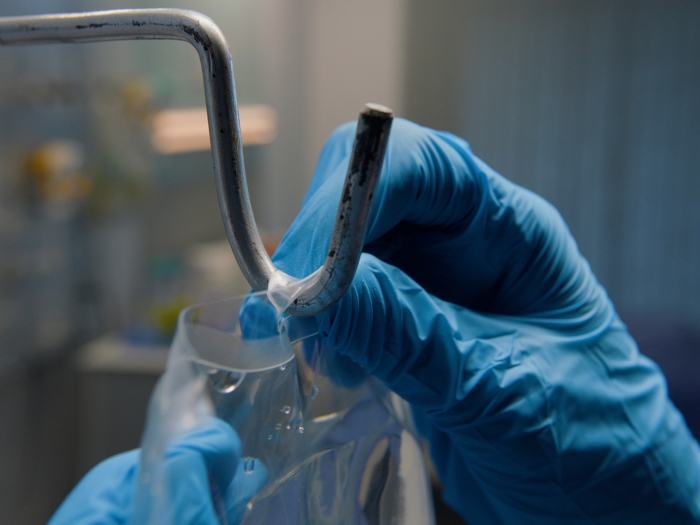
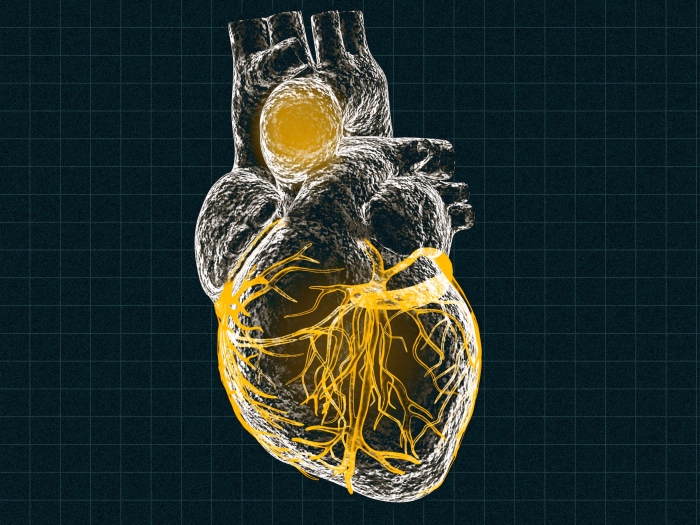
A team of researchers have spent the past eight years looking at better ways to transport organs for donation, specifically hearts, to improve the number of organs that can be used for transplants. They found that using a modified normothermic perfusion system heart preservation was feasible for up to 24 hours.

Health Lab
The newest version of the heparin reversal drug, described in a recent issue of Advanced Healthcare Materials, adjusted the number of protons bound to it, making the molecule less positive so it would preferentially bind to the highly negative heparin, resulting in a much safer drug.

Health Lab
A study reveals that what a doctor has behind them during a telehealth visit can make a difference in how the patient feels about them and their care.

Health Lab
A melanoma survivor shares facts and tips about preventing all types of skin cancer.

Health Lab
Young man with cystic fibrosis gets organ donation that changes his life

The Health Lab Podcast
Subscribe today on Apple Podcasts, Google Podcasts, Spotify, Stitcher or wherever you get your podcasts.
Health Lab
In emergency rooms and intensive care units across the country, clinicians make split-second decisions about which antibiotics to give a patient when a life threatening infection is suspected. Now, a study reveals that these decisions may have unintended consequences for patient outcomes.
Health Lab
Using human cells in an animal body, a team of researchers has developed a functional model of thoracic aortic aneurysm, creating opportunities for more effective understanding of disease development and treatments for the potentially fatal condition.

Health Lab
Recent developments represent a dramatic change from long standing federal policy around these substances that has historically criminalized their use and blocked or delayed research efforts into their therapeutic potential.

Health Lab
Building a comprehensive human kidney cell and tissue catalog could help develop more treatments for kidney disease.

Health Lab
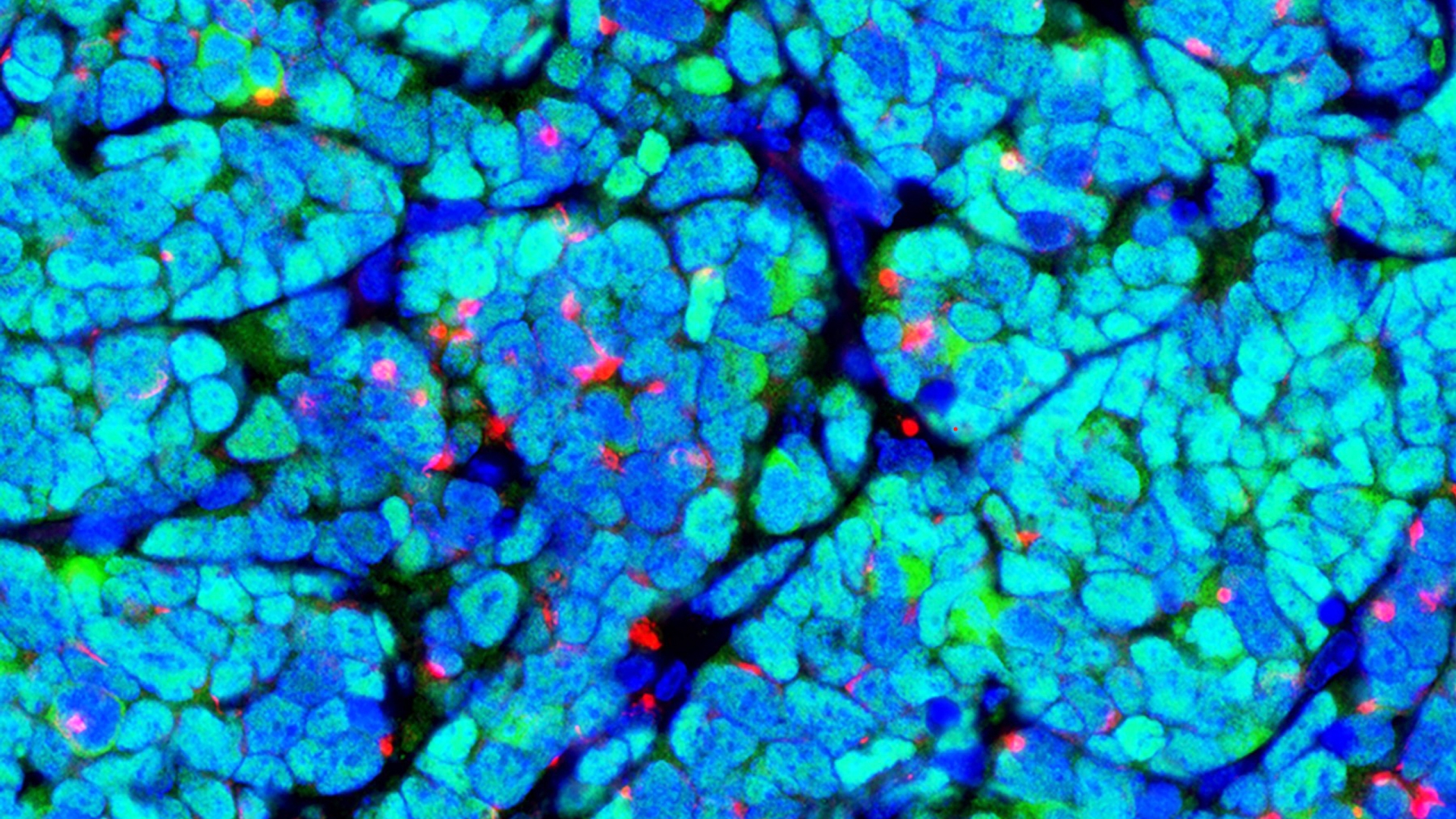
Experts in brain cancer outline current discoveries and offer a path of hope for glioblastoma treatment

Health Lab
Researchers improved memory and reduced neuroinflammation in a mouse model of Alzheimer’s Disease, suggesting another avenue for potential treatment.